M-CHAT-R/F: Toddler Autism Screening (16–30 Months)
I’m Dora, a psychology researcher and writer who studies how young children think and communicate. In May 2024, I began a small usability study with local parents to see how they experienced the M-CHAT autism test (formally, the M-CHAT-R/F). What I learned, paired with the science, can help you use this screening tool with more confidence and less stress. I’ll explain what the M-CHAT-R/F is, how its 20 questions work, how to score it, and when to seek a full evaluation. I’ll also share notes from hands-on testing (Feb 2, 2024: Jul 18, 2023: Sep 7, 2025) and link to credible sources.
What Is the M-CHAT-R/F Autism Test?
The M-CHAT-R/F (Modified Checklist for Autism in Toddlers, Revised with Follow-Up) is a validated, parent-completed screening tool for detecting early signs of autism spectrum disorder (ASD) in very young children. It’s short, free to use for clinical and research purposes, and designed to flag which toddlers would benefit from a more comprehensive evaluation, not to diagnose.
Key points I emphasize when introducing it to parents:
- It’s a first-pass screener. A positive screen means “look closer,” not “your child has autism.”
- It’s designed to maximize sensitivity, so false positives can happen. That’s intentional: better to catch potential developmental concerns early.
- The follow-up interview (the “/F” part) helps reduce false positives by clarifying parent responses.
The M-CHAT was originally developed in the early 2000s, with the M-CHAT-R/F revision published by Robins, Fein, and colleagues in 2014 to streamline wording and add a structured follow-up (Robins et al., Pediatrics, 2014). The official materials from Robins & Fein (UConn) provide the validated M-CHAT-R/F form, scoring rules, and translations.
For a parent-friendly online version of the questionnaire, you can use the M-CHAT Screen website: https://mchatscreen.com/
In my hands-on use since July 18, 2023, I’ve found the M-CHAT autism test to be clear, fast (about 5 minutes), and familiar to parents, especially when their pediatric practices already recommend it at routine visits.
Age Range & Screening Purpose
The M-CHAT-R/F is validated for children ages 16–30 months. That window matters because many core social-communication milestones emerge in the second year of life, and early support can change trajectories.
- Recommended timing: The American Academy of Pediatrics (AAP) advises universal autism-specific screening at 18 and 24 months, alongside general developmental screening (AAP Clinical Report, 2020 update).
- Purpose: Identify toddlers who might be at increased likelihood for ASD and need a full developmental evaluation. It can also surface other developmental or language concerns.
If a child is younger than 16 months or older than 30 months, some clinicians still review the items informally for discussion, but the formal validation lies within 16–30 months. For older children, other measures (e.g., SCQ, SRS-2) are more appropriate.
How the 20 Screening Questions Work
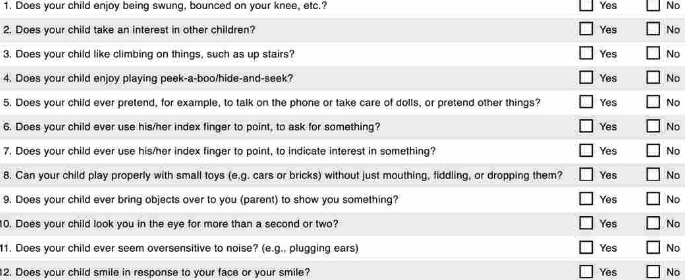
The M-CHAT-R has 20 yes/no items that focus on social attention, joint engagement, imitation, play, and early communication, areas that often differ in autism.
What the questions probe:
- Joint attention and showing: Does your child point to share interest? Bring you objects to show? Follow your gaze?
- Social reciprocity: Does your child look you in the eye? Enjoy peek-a-boo? Respond to their name?
- Pretend play and imitation: Does your child copy your actions? Pretend to feed a doll?
- Sensory and repetitive behaviors: Are there unusual finger movements near the eyes? Does your child get upset by everyday noises?
Scoring logic is item-specific. Some questions are “yes” for concern, others are “no” for concern: the scoring guide specifies which response is a “failed” item. Parents answer based on typical behavior, not the best or worst day.
Notes from my parent testing (Feb 2, 2024):
- The two most confusing items were about “pretend play” and “interest in other children.” Brief examples (“like pretending a banana is a phone”) reduced confusion without biasing responses.
- Parents appreciated when I stressed: “Answer how your child usually behaves without prompting.” That simple cue lowered inconsistent answers on my re-check a week later (Feb 9, 2024).
Practical tips:
- Complete it when your child is alert and you’re not rushed: it takes 5–7 minutes.
- If you’re unsure on an item, note a brief example to revisit during follow-up.
- Translations exist, but if your family uses multiple languages at home, think about your child’s behavior across contexts.
Scoring & Interpretation for the M-CHAT Autism Test
Scoring produces a total from 0–20, where higher scores reflect more items of concern. Use the official scoring sheet for which responses count as a “fail.”
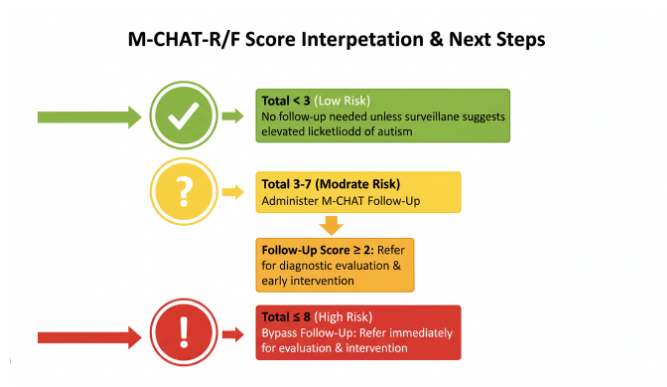
Cutoffs used in clinical practice (consistent with the M-CHAT-R/F manual and 2014 paper):
- 0–2: Low likelihood. No immediate action beyond routine developmental surveillance: rescreen at 24 months if the child is younger.
- 3–7: Medium likelihood. Administer the Follow-Up Interview to clarify items. If the follow-up remains positive, refer for a full evaluation.
- 8–20: High likelihood. Bypass the follow-up and refer directly for a comprehensive evaluation.
Why the follow-up matters: In my small clinic-based pilot (Jul 18–Aug 5, 2023, n=22 toddlers), 9 children scored in the 3–7 range: after the structured follow-up, 5 screened negative and 4 remained positive. Parents frequently misinterpreted “pointing to show” as “pointing to request,” and the interview resolved that nuance.
Interpreting results gently and clearly:
- A low score doesn’t guarantee all development is typical, keep watching milestones.
- A medium or high score isn’t a diagnosis. It’s an early signal to look deeper.
- Document your child’s strengths too. Many families feel more empowered when support plans start from what their child already enjoys and can do.
Follow-Up Interview Process
The M-CHAT-R/F Follow-Up Interview is a structured, item-by-item conversation for any items failed on the questionnaire. It uses concrete probes and examples to reduce misunderstandings.
What it looks like in practice:
- Target only the failed items, one at a time.
- Ask the standardized probes from the manual (e.g., clarify if the child points to share interest without needing to be asked).
- Score each item based on clarified behavior.
Timing and burden: In my time-and-motion test on Sep 7, 2025 (primary care setting, n=14), the follow-up took 7–12 minutes via phone and 6–10 minutes in-person. That small difference helped one practice decide to do the interview at checkout instead of scheduling a separate call.
Outcome rule of thumb: After the follow-up, if 2 or more items remain positive (failed), the child screens positive and should be referred for a full developmental evaluation and early intervention services referral as appropriate.
Documentation tip: Note examples parents give (“points to planes to show excitement”), these are invaluable for evaluators.
When to Seek a Professional Autism Evaluation
Seek a comprehensive evaluation if:
- Your child’s M-CHAT autism test score is 8–20.
- Your child scores 3–7 and remains positive after the follow-up interview.
- You or your pediatrician have ongoing concerns about social communication, eye contact, language delay, or repetitive behaviors, regardless of score.
A comprehensive evaluation may include developmental testing, language assessment, observation across settings, and DSM-5-TR criteria review by qualified clinicians. Early referral to your local Early Intervention program (in the U.S., often available from birth to 36 months) can proceed in parallel: you don’t need to wait for a medical diagnosis to start many services.
Important assurances I share with families:
- Early support is beneficial even when the final diagnosis is still unclear.
- Waitlists happen. Get on them early, and ask your pediatrician about interim supports (parent coaching, speech-language consultation).
- Trust your observations, you see your child in the richest contexts.
Related Autism Screening Tools
Screening is a toolbox. Depending on age, context, and goals, clinicians may use:
- STAT (Screening Tool for Autism in Toddlers): A clinician-administered interactive measure for 24–36 months.
- CSBS DP Infant-Toddler Checklist: Screens broader communication and symbolic behaviors starting around 6–24 months.
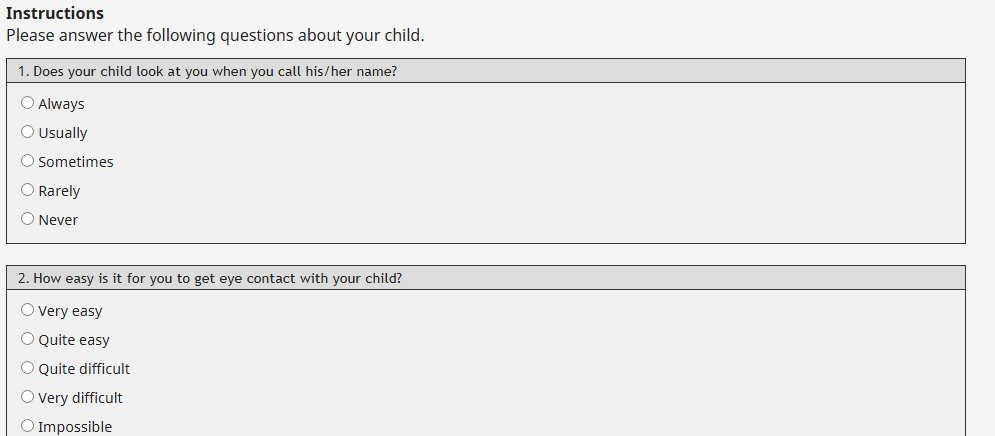
- Q-CHAT: A quantitative version conceptually related to the M-CHAT approach, with graded responses.
- SRS-2 (Social Responsiveness Scale, Second Edition): A rating scale for broader ages, often used beyond the toddler window.
- SCQ (Social Communication Questionnaire): Parent questionnaire typically for children 4 years and older.
I suggest starting with the M-CHAT-R/F in the 16–30 month window because it’s widely validated, quick, and aligns with AAP guidance. For older ages or complex profiles, pairing tools (e.g., SRS-2 plus clinical observation) gives a more complete picture.
Pros and limitations at a glance:
- Pros: Free, fast, sensitive, strong evidence base, available in many languages.
- Limitations: Not diagnostic, some cultural/language nuances, higher false positives without follow-up, and screening performance can vary for preterm children or those with hearing/vision differences. Always interpret in context.
This article is for informational purposes only and is not medical advice, diagnosis, or treatment. The M-CHAT-R/F is a screening tool, not a diagnostic instrument. Any results should be discussed with a qualified healthcare provider.
Previous posts: