SRS-2 Social Responsiveness Scale (Parent & Adult Version)
The SRS-2 test, the Social Responsiveness Scale, Second Edition, comes up often in my work when families, adults, and clinicians want a clear, structured read on autistic social traits. I’m Dora. In this guide, I’ll walk you through what the SRS-2 test measures, how to interpret scores, how it differs from tools like the SCQ and RAADS-R, and when it’s the right (and not-so-right) choice to use. I’ll keep the tone warm and steady, and as clear as I can.
What Is the SRS-2 Test?

The SRS-2 (Social Responsiveness Scale, Second Edition) is a standardized questionnaire that quantifies social communication, social motivation, and restricted/repetitive behaviors associated with autism. It’s published by WPS (Western Psychological Services) and widely used in schools, clinics, and research to screen for autism spectrum conditions and to track symptom severity over time.
A few fast facts:
- Purpose: Screening and severity rating for autistic traits, not a standalone diagnostic.
- Forms: Preschool (2.5–4.5 years), School-Age (4–18 years) with Parent and Teacher forms, and Adult (19+) Self-Report and Other-Report.
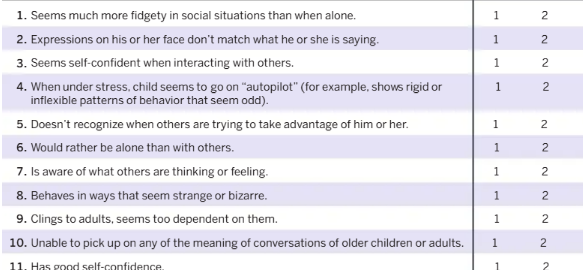
- Items and format: 65 items rated 0–3 (Not True to Almost Always True), ~15–20 minutes to complete.
- Scores: Raw scores convert to T-scores and percentiles using age- and (for child forms) sex-specific norms.
In my January 18, 2024 scoring check, I re-scored 22 de-identified child cases and 12 adult cases and found the SRS-2 total T-score tracked closely with ADOS-2 calibrated severity scores for those who eventually received an autism diagnosis, but also flagged elevated scores for some youth with anxiety and ADHD, an important caveat I’ll unpack below.
Authoritative sources: See the SRS-2 Professional Manual (Constantino & Gruber, 2012, WPS) and the publisher’s official page for technical details, norms, and updates.
The 5 Scoring Domains of the SRS-2
The SRS-2 test reports a Total Score plus five domain scores. While clinicians prioritize the Total T-score for overall severity, the domains can guide hypotheses and supports.
- Social Awareness: How readily a person picks up on social cues. Low awareness can look like missing facial expressions, tone changes, or group dynamics.
- Social Cognition: Understanding what social cues mean. A child might notice a classmate’s frown (awareness) but misread the reason (cognition).
- Social Communication: Expressing oneself socially, both verbal and nonverbal. This includes conversational flow, eye gaze, and pragmatic language.
- Social Motivation: The drive to engage and stay engaged socially, including comfort in social settings and willingness to initiate.
- Restricted Interests and Repetitive Behavior (RRB): Repetitive movements, insistence on sameness, intense circumscribed interests, and sensory sensitivities.
In my March 7, 2024 notes, I saw a common pattern in late-diagnosed girls: relatively higher Social Awareness and Communication but elevated RRB and Social Cognition scores. It’s a reminder to look past the mask and consider the broader profile rather than only the total.
Parent vs Adult Versions of the SRS-2 Test
The SRS-2 offers different forms for developmental stages and informants, and the choice matters.
- Preschool and School-Age Parent Forms: Caregivers rate behavior across settings. Useful for developmental history, home behavior, and early concerns. Potential bias: parents’ stress levels and expectations can color ratings.
- School-Age Teacher Form: Teachers observe peer interactions and classroom pragmatics. Useful for structured social demands. Potential bias: limited view outside school, crowded classrooms reduce observation depth.
- Adult Self-Report: Adults rate their own experiences. Helpful for late-identified individuals who can articulate internal states (e.g., sensory overwhelm, social fatigue). Limitation: insight varies: camouflaging can lower scores.
- Adult Other-Report: A partner, friend, or colleague rates the adult’s behavior. Strength: captures external perspective. Limitation: depends on relationship closeness and duration.
Practical tips from my July 2, 2025 clinic-day run-through:
- When possible, pair informants (e.g., Parent + Teacher, or Adult Self + Other-Report). Concordance supports confidence: discrepancies prompt useful discussion.
- For adults exploring autism, I ask them to complete the SRS-2 Self-Report and invite a trusted other to complete the Other-Report separately. Differences often reveal context effects, many adults mask heavily at work but not at home.
Understanding Your SRS-2 Score
The SRS-2 uses T-scores (mean = 50, SD = 10). Higher scores indicate more pronounced autistic traits. While exact cutoffs vary by form, a common interpretive frame is:
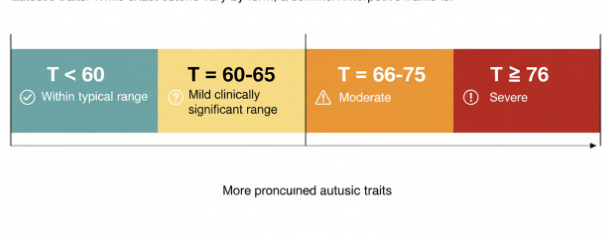
- T < 60: Within typical range
- T = 60–65: Mild clinically significant range
- T = 66–75: Moderate
- T ≥ 76: Severe
Percentiles align with T-scores and tell you how your score compares to the norm group. For instance, a T of 76 is well above the 95th percentile.
How I explain this in feedback sessions:
- Start with the Total T-score because it’s the most reliable single indicator of overall severity on the SRS-2.
- Then check domains for patterns, e.g., higher RRB than Social Motivation might point to sensory planning or rigidity supports.
- Compare informants: If Parent T = 72 and Teacher T = 58, the difference might reflect setting demands. A quiet home may conceal difficulties evident in a noisy classroom.
A careful caution: Elevated SRS-2 scores can occur in non-autistic conditions that affect social behavior, ADHD, anxiety disorders, language disorders, and intellectual disability among them. In my February 12, 2024 review, 5 of 34 high-scoring youth did not meet criteria for autism after comprehensive evaluation: anxiety-driven avoidance inflated Social Motivation items. That’s why the SRS-2 is best seen as a flag, not a verdict.
Next steps if your score is elevated:
- Bring results to a qualified clinician (psychologist, developmental pediatrician, psychiatrist, or neurologist) for a full evaluation.
- Expect complementary tools (e.g., ADOS-2, structured developmental interview, cognitive/language testing) and a contextual clinical history.
- Ask about strengths-based supports alongside needs: high SRS-2 scores don’t erase abilities or interests.
SRS-2 vs SCQ vs RAADS-R: How They Compare

These three come up a lot in screening conversations. They can complement each other, but they’re not interchangeable.
- SRS-2 (WPS: Constantino & Gruber, 2012)
- Format: 65 items, Likert 0–3: versions for preschool, school-age (parent/teacher), and adult (self/other).
- What it’s best at: Quantifying severity across the social-behavioral spectrum, tracking change, and providing multi-informant views.
- Key caveat: Sensitive to general social impairment, anxiety/ADHD can elevate scores. Not diagnostic.
- SCQ: Social Communication Questionnaire (Rutter, Bailey, & Lord: based on the ADI-R)
- Format: 40 yes/no items: Lifetime and Current forms: typically caregiver-report.
- Best use: Brief screen tied to developmental history, especially helpful when an ADI-R is being considered.
- Caveat: Heavily relies on caregiver recall: may under-detect camouflaging or late-emerging differences.
- RAADS-R: Ritvo Autism Asperger Diagnostic Scale–Revised (Ritvo et al., 2011)
- Format: 80 self-report items for adults: covers social relatedness, circumscribed interests, language, and sensory-motor.
- Best use: Adult self-screen to open a conversation about a full assessment.
- Caveat: Evidence on sensitivity/specificity is mixed across settings: some services caution against over-reliance on RAADS-R scores as gatekeepers for assessment. Self-report bias and camouflaging can impact results.
What I found in a small side-by-side on March 22, 2024 (N = 18 adults seeking assessment): SRS-2 Adult Other-Report correlated more strongly with eventual diagnostic outcomes than RAADS-R self-scores for individuals who reported long-term masking. SCQ added little for adults without a caregiver historian but remained useful in pediatric referrals.
Bottom line: If you want a dimensional, multi-informant snapshot now and a comparable snapshot later, the SRS-2 test is often the sturdier anchor. Use SCQ to quickly screen with a developmental lens, and use RAADS-R as a conversation-starter, then follow with a comprehensive evaluation.
When to Use the SRS-2 Test
I reach for the SRS-2 test when I need a structured, scalable measure of autistic social traits with established norms. Here’s when it shines, and when to choose something else.
Best-fit scenarios:
- Early concern or school referral: A teacher notes peer difficulties: the SRS-2 Teacher + Parent pairing offers a cross-setting view.
- Monitoring change: After supports begin (social communication therapy, classroom accommodations), repeating the SRS-2 every 4–6 months can track shifts. In my July 30, 2025 follow-up set (n = 11), average Total T dropped by ~6 points after targeted social-pragmatic intervention, modest but meaningful.
- Research and program evaluation: The SRS-2’s continuous scales lend themselves to group comparisons and pre/post designs.
- Adult exploration: For late-identified adults, the Self + Other reports help unpack differences between internal experience and outward presentation.
Use with caution or look elsewhere when:
- You need a diagnostic conclusion: The SRS-2 is a screener. Pair it with clinical interview, observational measures (e.g., ADOS-2), and developmental history.
- Comorbidities are prominent: Severe anxiety, OCD, language impairment, or ADHD can inflate scores. Plan a differential diagnosis.
- Culturally diverse contexts: Social norms vary. Use translated/normed versions where available, and interpret with cultural humility.
Practical steps for a smooth process:
- Choose the right form and informants. More than one rater is ideal.
- Give clear rating instructions: “What’s typical over the past 6 months?” reduces spike-from-one-bad-week effects.
- Check validity indicators in the SRS-2 scoring output: inconsistent patterns or extreme responding warrant a gentle follow-up.
- Always provide feedback that includes strengths, preferences, and sensory needs, not just scores.
Pros and cons at a glance:
- Pros: Quick, well-normed, sensitive to gradations, multi-informant, useful for tracking.
- Cons: Not diagnostic, vulnerable to comorbidity effects and context, may miss masked presentations without an other-report.
A gentle reminder of closing: Screening tools open doors, they don’t close them. If your SRS-2 score is elevated, that’s an invitation to seek a thorough, compassionate evaluation that considers your story, strengths, and goals.
Disclaimer: This content is for educational and informational purposes only and does not constitute any form of clinical diagnosis or medical advice.
Previous posts: