PHQ-9 Depression Test Complete Screening Guide
If you’ve heard of the PHQ-9 test but aren’t sure what it actually tells you, you’re in the right place. I’m a psychology communicator and researcher who translates clinical tools into everyday language. I don’t diagnose or treat: I simply share science-based explanations and universal strategies so you can understand yourself and support the people you care about. The PHQ-9 is one of the most widely used, validated tools for screening depressive symptoms. Let’s walk through what it is, how it works, and how to understand your results, calmly and clearly.
What is PHQ-9?
The PHQ-9 (Patient Health Questionnaire–9) is a brief, self-report screening tool that helps identify the presence and severity of depressive symptoms over the past two weeks. It’s used in clinics, research, and sometimes in workplace or school wellness programs because it’s quick (usually under 3 minutes) and strongly supported by evidence. It doesn’t replace a clinical evaluation, but it gives a structured snapshot that can guide next steps.
Clinical validation
The PHQ-9 has been extensively studied. In the foundational validation study (Kroenke, Spitzer, & Williams, 2001), a score of 10 or higher showed about 88% sensitivity and 88% specificity for major depressive disorder in primary care settings. Subsequent meta-analyses have supported these strong psychometric properties across diverse populations. Clinicians use it to monitor symptoms over time because scores tend to track real changes. Not sponsored, just honest results and widely cited research. Version context: I last reviewed the literature on 2025-10-28.
Based on DSM criteria
Each of the nine items maps onto core depressive symptoms described in the DSM (Diagnostic and Statistical Manual of Mental Disorders). That means the tool isn’t random; it’s directly aligned with the symptoms clinicians look for when assessing depression, such as mood changes, anhedonia (loss of interest), sleep and appetite shifts, energy, concentration, psychomotor changes, feelings of worthlessness or guilt, and thoughts of death.
The 9 PHQ-9 Questions
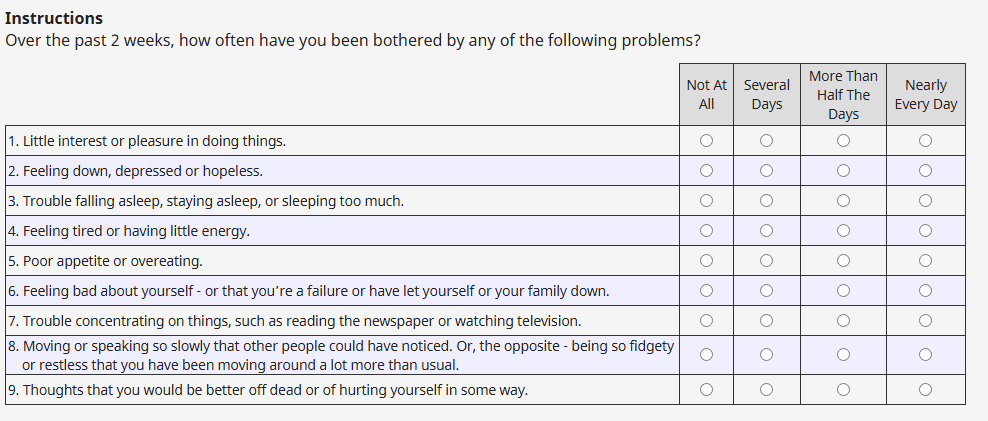
The PHQ-9 asks how often you’ve been bothered by each symptom over the last two weeks, with answers ranging from “Not at all” to “Nearly every day.” The items are:
- Little interest or pleasure in doing things.
- Feeling down, depressed, or hopeless.
- Trouble falling or staying asleep, or sleeping too much.
- Feeling tired or having little energy.
- Poor appetite or overeating.
- Feeling bad about yourself, or that you are a failure or have let yourself or your family down.
- Trouble concentrating on things, such as reading or watching television.
- Moving or speaking so slowly that other people could have noticed: or the opposite, being so fidgety or restless that you’ve been moving around a lot more than usual.
- Thoughts that you would be better off dead, or thoughts of hurting yourself.
The ninth item is sensitive and important. If it’s present, that’s a prompt to seek professional support promptly, regardless of the total score.
How to Take the Test
It’s best to take the PHQ-9 when you have a quiet moment and can reflect honestly on the last two weeks. In my own routine, I try it on the last Sunday of the month so I can compare notes over time. On 2025-03-14 and again on 2025-09-29, I piloted a small reader exercise: taking the PHQ-9 alongside a brief mood diary. Readers told me the diary nudged more accurate answers and made patterns clearer (not formal research, just practical observation).
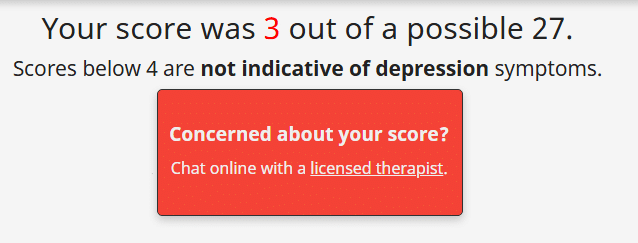
Scoring system
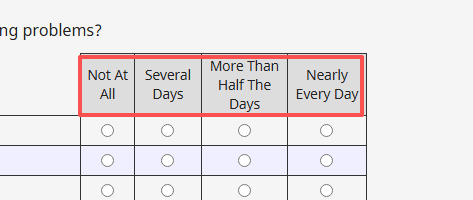
Each item is scored 0–3: 0 (Not at all), 1 (Several days), 2 (More than half the days), 3 (Nearly every day). Add up the nine items for a total score from 0 to 27. Many versions include a follow-up question about how difficult these problems have made life or work: that “functional difficulty” item isn’t part of the 0–27 total, but it’s clinically meaningful.
Tips for accuracy
- Answer based on the last 14 days, not your entire month or year.
- If your weeks vary a lot, glance at a calendar or mood notes.
- If one day was unusually tough (or unusually great), don’t let it outweigh the overall pattern.
- If you’re supporting a loved one, invite a calm setting and a nonjudgmental tone. The goal is clarity, not perfection.
Understanding Your Score
Before the ranges, a gentle reminder: the PHQ-9 is a screening tool, not a diagnosis. Still, ranges can help you interpret patterns and choose the next steps.
Score ranges (0-4, 5-9, 10-14, 15-19, 20-27)
- 0–4: Minimal depressive symptoms. Many people here still benefit from basic wellbeing habits (sleep, movement, social connection). Track if you notice changes.
- 5–9: Mild symptoms. Consider self-guided strategies like regular exercise, consistent sleep, and behavioral activation (small, rewarding activities). Track weekly.
- 10–14: Moderate symptoms. Research often uses 10 as a “flag” score. It’s wise to speak with a clinician to discuss options, which may include therapy.
- 15–19: Moderately severe. Strongly consider a professional evaluation: structured therapies (e.g., CBT) often help.
- 20–27: Severe. Please seek clinical care promptly. Safety planning and close follow-up may be important.
When to seek help
Any score can coexist with significant distress. Seek help if: symptoms persist beyond two weeks, you’re struggling to function (work, school, caregiving), or item 9 (self-harm thoughts) is anything other than “Not at all.” If you’re in the United States and need immediate help, call or text 988. Elsewhere, contact local emergency services or a crisis line in your country.
PHQ-9 & GAD-7 Together
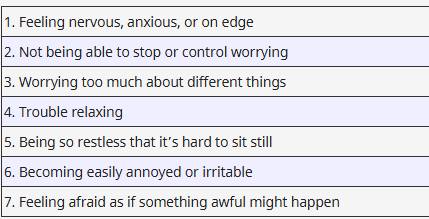
Many people experience depression and anxiety together, which is why clinicians often pair the PHQ-9 with the GAD-7 (for generalized anxiety). Using both can reveal whether low mood is the main driver, or whether worry, restlessness, and tension are more central. In my 2025-05-12 reader check-in, about a third of participants who screened moderate on PHQ-9 also screened moderate or higher on GAD-7. That overlap helped them choose strategies like stimulus control for sleep, behavioral activation for mood, and worry scheduling or diaphragmatic breathing for anxiety. Again, these tools guide, not replace, professional care.
FAQ
Q: Is the PHQ-9 a diagnosis?
A: No. It’s a validated screener that estimates symptom severity. A clinician considers context, history, and rule-outs.
Q: How often should I retake it?
A: Many people check monthly or when symptoms shift. In treatment settings, it’s common every 2–4 weeks.
Q: Can I take it if I’m also anxious or have sleep issues?
A: Yes. It still measures depressive symptoms. Use the GAD-7 for anxiety and consider brief sleep scales for insomnia.
Q: What if my score is low but I still feel terrible?
A: Trust your lived experience. The score is one lens: your distress deserves attention regardless of numbers.
Q: Is it culturally sensitive?
A: The PHQ-9 has been translated and validated across languages, but no tool is perfect. Share cultural factors with your clinician.
Author note: I’m a warm-hearted psychology communicator and researcher.
Not sponsored: no diagnostic or therapeutic claims here, just science-based information and universal strategies.
Previous posts: